In this ongoing series, we analyze the recently released Medicare physician payment database to identify wasteful spending by Medicare and seniors, including on treatments proven to be ineffective or in cases where equally effective alternatives to a high-priced treatment exist.
A growing controversy in medical circles concerns the treatment of prostate cancer with proton beam radiation therapy. This relatively new treatment, used on a variety of cancers, is provided in specially constructed facilities costing hundreds of millions of dollars. In order to recoup these hefty construction costs, proton therapy centers aggressively promote their services for a broad array of cancers, especially the relatively common prostate cancer. However, there is currently zero evidence that proton radiation therapy is more effective for treating prostate cancer than the alternative standard treatment, which is half the cost. With the number of proton therapy centers in the United States expected to double in the next few years, Medicare and seniors face the prospect of rapidly increasing prices for prostate cancer treatment, with no proven benefits for beneficiaries.
Background
To date, studies have consistently shown proton radiation therapy, or PRT, to be no more effective in treating prostate cancer than intensity-modulated radiation therapy, or IMRT, the dominant treatment alternative that costs half what PRT does. IMRT is a widely used, advanced version of radiation therapy. PRT is a newer radiation technology that uses positively charged particles known as protons. In certain cases—primarily for cancers in children and in sensitive regions such as the spinal cord—PRT improves safety by lowering the degree of toxicity to which the surrounding tissue is exposed. However, for other cases, including prostate cancer, PRT offers no improvement over IMRT. Multiple studies have been unable to demonstrate any added clinical benefit of PRT over IMRT for prostate cancer, and one recent study indicated no difference between the two in toxicity in prostate patients 12 months after treatment. Yet despite this lack of apparent clinical benefit, almost 80 percent of Medicare’s spending on PRT goes toward prostate cancer treatment. This substantially increases the cost of treatment for Medicare and seniors, since the median Medicare reimbursement for PRT is about 1.7 times higher than that for IMRT.
Despite these concerns, the United States currently has 14 operational PRT centers, with at least 12 more under construction or in development. These facilities cost anywhere from $125 million to more than $200 million to build and are roughly the size of a football field. By 2017, they are expected to garner $1.17 billion in annual revenue. The question relevant to taxpayers, Medicare, and seniors, then, is where the PRT centers will find this revenue. By one estimate, a $125 million center must treat 2,000 patients per year and generate more than $50 million in annual revenue to turn a profit. Although PRT is recognized as a preferred option for treating children and some specific cancers, these cases are not prevalent enough to fill the necessary spots in centers. Thus, proton therapy centers have aggressively advertised their services for prostate cancer and other more common forms of cancer to maximize their revenue potential. Given these incentives, the cost of PRT to Medicare will only grow over time, even in cases where no medical basis for selecting PRT exists. Already, prostate patients range from 10 percent to more than 50 percent of some proton therapy centers’ caseloads and represent 79 percent of Medicare’s spending on proton therapy treatment.
Potential savings to Medicare and seniors
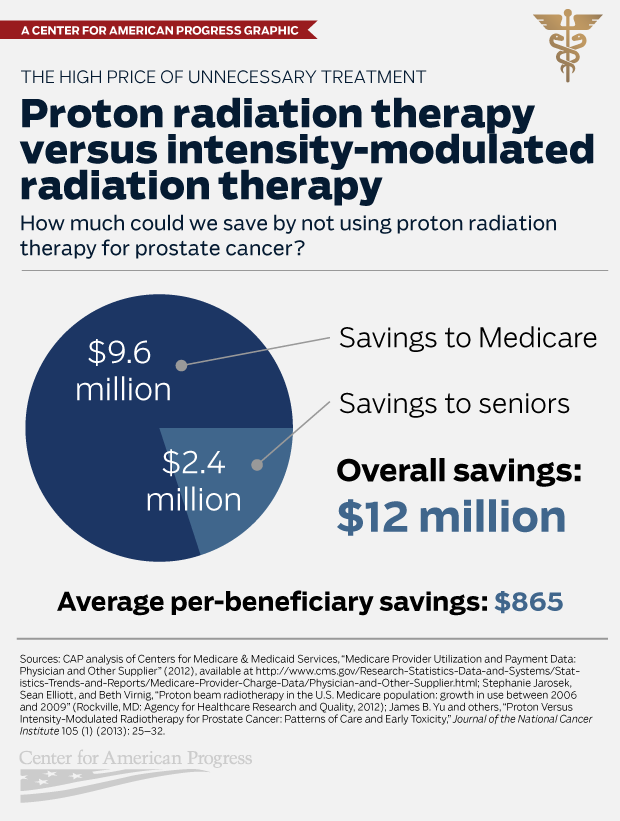
Medicare spent an estimated $22.4 million on proton beam radiation therapy for prostate cancer in 2012. If IMRT had been used to treat all of these cases, Medicare would have spent only $12.8 million—saving $9.6 million.
Medicare beneficiaries, meanwhile, would have saved an additional $2.4 million in out-of-pocket costs such as co-insurance. While the Medicare payment database does not include patient data, it does indicate that 3,506 unique Medicare beneficiaries received proton beam radiation therapy. If all beneficiaries received the same level of IMRT treatment, savings would average $685 per senior. The exact level of savings per senior would depend on the doses received by each beneficiary; while many seniors have supplemental coverage that covers co-insurance, premiums for this coverage would be lower if it did not have to cover proton beam radiation therapy costs.
Savings to Medicare and beneficiaries combined would have totaled about $12 million in 2012.
Methodology
The Medicare payment database does not include diagnosis information, so we used a Department of Health and Human Services analysis to estimate the percent of Medicare’s proton beam radiation spending that went toward prostate cancer treatment—79 percent. In addition, the Medicare database’s billing codes correspond to specific dose levels of both PRT and IMRT that may not be directly comparable. To work around this, we divided overall Medicare spending on PRT by the average Medicare payment amount for the treatment, as calculated by a 2011 study. IMRT’s median reimbursement was $18,575, and PRT’s was $32,428. These prices include beneficiary cost sharing—set at 20 percent of a treatment’s cost—so we reduced these prices by 20 percent to isolate the price paid by Medicare.
Dividing Medicare spending on PRT for prostate cancer by the median price paid by Medicare gave us an estimate of the number of treatments, which we multiplied by the IMRT price to find the cost of treating these patients with IMRT. We subtracted this cost from the proton beam radiation spending for prostate cancer to estimate the potential savings from switching to IMRT for these patients. Since this only represented Medicare savings, we then calculated the value of the additional 20 percent to find beneficiary savings.
Conclusion
Proton radiation therapy is a prime example of our health system rushing headlong into an unproven, costly treatment. Medicare wisely lowered its reimbursement amount for PRT in 2013 in order to reduce the perverse incentives that have encouraged the proliferation of PRT for cancers for which it offers no added benefit. Nevertheless, as the number of expensive proton therapy centers remains on track to double in the next few years, PRT poses a growing risk for a greater waste of taxpayer money.
Topher Spiro is the Vice President for Health Policy at the Center for American Progress. Thomas Huelskoetter is the Special Assistant for Health Policy at the Center. Gina Phillipi was formerly an intern on the Health Policy team at the Center.
The Center for American Progress thanks the Peter G. Peterson Foundation for its support of our Health Policy programs and of this fact sheet. The views and opinions expressed in this fact sheet are those of the Center for American Progress and the authors and do not necessarily reflect the position of the Peter G. Peterson Foundation. The Center for American Progress produces independent research and policy ideas driven by solutions that we believe will create a more equitable and just world.